
Professor Karen Hoare.
Alongside her role as Massey’s Director of Postgraduate Nursing, Professor Hoare is a partner and current Chief of Staff at Greenstone Family Clinic in Manurewa. Here, she specialises in caring for mothers, babies, and young people, and works with the Greenstone team to implement systems that prevent vulnerable patients going unnoticed. In the past two years, she has been working on the frontline of the COVID-19 pandemic.
Professor Hoare says the various hats she wears creates a synergy that demonstrates the importance of partnering academic knowledge with clinical practice in the nursing environment.
“It’s important for me to still be practicing at the clinic because it keeps me grounded so I know exactly what’s going on in primary healthcare. Everything I do clinically informs my teaching, as well as my on-going research. It’s all connected and strengthened because of it. I really believe in the power of pairing academic with clinical because nurses lead, they make a difference, and they’ve demonstrated it throughout the pandemic especially.”
Professor Hoare joined Massey in 2017, and accepted the role of Director the following year. Her role includes overseeing the postgraduate courses and promoting postgraduate nursing. She says while the nurse practitioner pathway is growing, there’s still a long way to go.
“On last check, we had 617 nurse practitioners. I want to see that number keep increasing, especially more Māori and Pasifika nurse practitioners. Our school is training future health care leaders with a focus on improving primary health care, mental health, child and youth health care, and the health of our older population.”
A nurse practitioner is an advanced nurse who has the same legal authorities as doctors to prescribe, to diagnose, and to offer a whole package of care. Professor Hoare says the journey can be tough, but through team effort, students are supported the entire way.
“The faculty that I work with, the nurse practitioners and all the postgraduate coordinators, work hard and are a really great team. We want to make sure that we’re giving the students the very best experience and that comes from having expert teaching leaders.”
Part of Professor Hoare’s role is to oversee the final year programme for nurse practitioners. She manages, teaches, and provides mentorship to the candidates working towards nurse practitioner registration.
“I’ve had a fabulous time as a nurse, doing research, doing teaching – now I’m mentoring the next generation. It’s important to work closely with our nurse practitioner candidates in that final year because we want to make sure they’re ready. If we feel they’re not ready to face the Nursing Council for their panel assessment, then we advise them and let them know we’re right there with them on the same team to support their success.”
Professor Hoare’s other great passion is children and youth health. At 18, she trained to be a registered nurse at Great Ormond Street Hospital in London, the world’s second oldest children’s hospital with the motto ‘the child first and always’. She says she’s carried this mantra throughout her career, and it helped her build Greenstone Family Clinic in the image of the hospital that educated her.
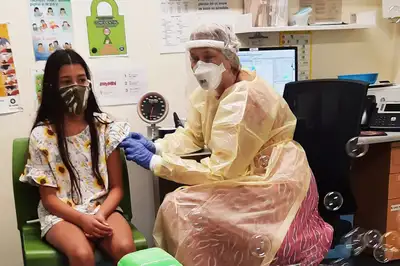
Professor Hoare vaccinating a 10-year-old during the COVID-19 immunisation rollout.
“Paediatrician Dr Charles West established Great Ormond Street in 1852 with the following objectives: to train paediatric nurses, to conduct research to benefit children, and to provide healthcare for the impoverished children in the East End of London. Looking at what we do at Greenstone – we do research, we’re a teaching practice so we train nurses, nurse practitioner candidates and medical students, and we provide free healthcare for children. I’d like to see more of what we do modelled around the rest of the country.”
In 1989, Professor Hoare had the opportunity to travel to The Gambia which she says was massively formative for her and her career. She’d previously completed a Diploma of Health Visiting, which encompassed a specific health role in the United Kingdom that focused on epidemiology.
“My husband, who is a paediatrician, was sent to the Medical Research Council Facilities in The Gambia, and I went with him. They’d never had a health visitor in the unit before, but I was able to investigate the types of diseases children succumbed to and how to mitigate these through community development and spreading health promotion to improve health literacy. My husband supported me to learn more advanced assessment skills to alleviate his workload as he was so busy, which started me on the whole advanced clinical role.”
The following two years saw Professor Hoare leading a quasi-experiment to measure the effectiveness of the health education programme she’d established. She says she was inspired to start the programme after seeing a nine-month-old baby die because her mother didn’t understand the role of oral rehydration solution in treating diarrhoeal disease.
“There was a dearth of knowledge in the village about hygiene and infant health care. An eight-week rolling health education programme was devised which involved weekly one-hour discussions centred on childcare topics such as immunisations, weaning, serious illness, and hygiene. In 1997, six years after the project ended, I returned to The Gambia to examine long-term trends and found the project had caused a huge reduction in hygiene-related childhood infections across the village.”
Professor Hoare attributes this time as the start of her academic career, which motivated her to study for a Master of Health Sciences degree and then her PhD a decade later.
After migrating to Aotearoa New Zealand at the end of 2003, Professor Hoare began working as a public health nurse and found the health services available for children at the time needed serious improvement. She says she needed to find a way to continue in a clinical role and to demonstrate what a United Kingdom trained paediatric nurse and health visitor could do.
“I was frustrated after coming to New Zealand and found it hard to find a career path. If it hadn’t been for Professor Bruce Arroll from the University of Auckland, who supported me when I asked if I could run a nurse-led children’s clinic at Greenstone, I’d have gone back to England. Six months into running that clinic, I was encouraged to become a nurse practitioner which led me to where I am today.”
Her research remains focused on improving the lives of children. She says they are the biggest health promoters.
“I’m currently working on an obesity project which focuses on bringing children in, getting them to set goals for themselves, and making a change through challenging their parents. It’s a powerful way to instil better health practices for the whole whānau – by starting with the children. One of my favourite quotes is: ‘If you want to achieve the impossible, give it to the young because they don’t know it can’t be done’.”
While still a few years away, Professor Hoare’s next big adventure is retirement. With family across the world, including three adult children and her first grandchild, she’s planning on being just as busy as she has been across her career.
She says she hopes to leave the academic door open for more nurse practitioners to find their way forward.
“I’m currently the only nurse practitioner who is also a professor, and I need someone to take on the mantle. I’m proof that it can be done – nurse practitioners are expert nurses, so they need to keep up to date. You never stop learning, and you never should stop learning. Especially in nursing because things change all the time.
“To those considering becoming a nurse practitioner, just do it because it’s such a wonderful job. I think my experience demonstrates how varied your career can be, and what a fantastic career I’ve had. Don’t ever let people say you can’t do it.”
Related news
Massey staff recognised at Primary Healthcare Awards
Maria Kekus and Associate Professor Karen Hoare have been named category winner and finalist respectively at the recent Primary Healthcare Awards.

Industry collaboration reimagines new era for older persons’ healthcare
The Massey University School of Nursing recently co-hosted the National Oceania Clinical Leaders symposium, alongside Oceania Healthcare. The symposium took place on International Nurses Day on 12 May.

Holistic approach to nursing comes full circle
The road to become a mātangi tapuhi (nurse practitioner) has been a long but exceptional one for Kate Te Pou, spanning more than two decades.
