3,553 women involved
These were exclusively Māori, Pasifika, or Asian women, who are at higher risk from cervical cancer or of being under screened.
HRC funding
Health Research Council funded trials, as well as other bodies.
Clear-cut conclusion
Yes / No setup means findings are ready for implementation in Aotearoa.
2023 roll-out
Government has agreed to make self-testing available from July 2023.
When Doctor Naomi Brewer started her PhD on demographic differences in cervical cancer survival back in 2007, she knew cancer rates were higher for Māori and Pasifika communities. But she didn’t know why this was the case. No one did.
At the time, there was "not a lot of information on the specifics of why that might be the case," Brewer recalls. "My PhD was looking at demographic differences in cervical cancer survival … It was mainly about ethnicity, but it included other factors."
Brewer’s research — in her doctorate and in subsequent projects — set out to solve this real-world problem and is leading to practical solutions.
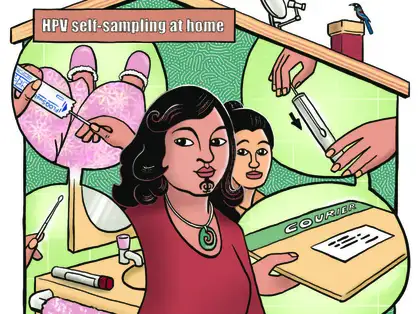
Brewer and her research team adopted and adapted an internationally trialled medical HPV intervention for Aotearoa: culturally appropriate, mana-enhancing self-testing swab kits for Māori, Asian, and Pasifika women to use in the comfort and privacy of their own homes.
Read Doctor Naomi Brewer's PhD paper
Read New Zealand Medical Journal article about self-testing pilot
Watch One News Coverage, interviewing cervical health advocates about test
Cervical cancer and HPV
In Aotearoa, about 160 women develop cervical cancer each year – and about 50 die from it. Human papillomavirus, or HPV, causes 95 per cent of cervical cancer.
Those at higher risk of cervical cancer can be identified early by detecting HPV and, if HPV is found, then followed up with direct examination. This means we have the rare opportunity to seriously reduce, if not entirely eradicate this type of cancer in women, especially as we now have more and more young women in the population who are vaccinated against HPV.
Human papillomavirus — Ministry of Health
Māori and Pasifika women at higher risk
Brewer’s PhD research found that a multitude of inter-related factors — from cultural norms to screening rates — combined to make Māori and Pasifika women more vulnerable to cervical cancer overall.
"The main finding was there was no one single causal factor," Naomi explains. Instead, multiple 'minor' factors all contribute to higher risks: Māori and Pasifika women don’t get screened as much.
Travel time to a doctor was an additional contributing factor. Overall, rural women are more at risk of cervical cancer, regardless of ethnicity. But a higher proportion of Māori women live rurally, meaning they are less likely to get tested, which — once again — heightens their risk of developing cancer.
"The main finding was there was no one single causal factor."
When Brewer completed her PhD in 2011, she had the good fortune to land Professor John Potter — one of Aotearoa’s most prominent public health researchers — as a thesis examiner. Potter was impressed with Brewer’s work and could immediately see its potential applications.
"This is really important work", Potter remembers thinking to himself as he read it. "It opened the door to say: there isn't a quick fix for this problem. There's a whole bunch of factors, to do with deprivation, with access, with socio-economic status generally. And then there’s the important cultural and gender aspects – which Naomi Brewer spent time on."
"I want to be sensitive to women's needs — it's the whole point of my research really," Brewer agrees.
"I want to be sensitive to women’s needs — it’s the whole point of my research, really."
Navigating whakamā and distrust
Brewer explains a woman’s genital region is considered sensitive and private in most cultures — hence the Western term ‘private parts’. For Māori and Pasifika women it can go further; for many, their genitals are tapu (sacred). This means Māori and Pasifika women are likely to experience whakamā (shyness, shame) at the prospect of a doctor or nurse — and especially a stranger — seeing them with their legs wide open, then putting a speculum into a private and tapu part of their body.
"Wāhine and Pasifika women may have had a bad experience with doctors or with a previous smear," Brewer clarifies. "Pap smears are often painful, too. So if you’ve gone to the clinic, you’re already feeling embarrassed, you’re worried about it being tapu, it’s painful, and then the doctor or nurse doesn’t treat you very well — what’s the incentive to go back?"
"Wāhine Māori and Pasifika women may have had a bad experience with doctors, or with a previous smear."
Worldwide, cervical cancer is the fourth leading cause of cancer death, leading to approximately 300,000 deaths per year. Although cervical cancer might not seem like a ‘big’ problem in Aotearoa New Zealand – approximately 50 women die from it every year in this country – this relatively low number is due to the success of our immunisation, screening, and treatment processes.
Meanwhile, Potter points out that "Māori women have a mortality rate that’s two and a half times higher than the rest of the population."
Māori and Pasifika communities have high levels of distrust in the New Zealand health system, and good reasons for this distrust, starting with the trauma of colonisation itself. This suspicion manifests in many ways, including reluctance to visit hospitals and doctors, and lower vaccination rates.
"Māori women have a mortality rate that’s two and a half times higher than the rest of the population."
Self-testing Porirua pilot
In 2011, Brewer started noticing an increase in articles proposing novel self-testing procedures. This is where women take swabs from their own vaginas, then send the samples into a doctor or medical clinic. Among these, a major article in the British Journal of Cancer, distributed by leading academic publisher Nature.
Brewer teamed with Potter and they put together a research team to start working on a plan to trial self-testing for HPV in Aotearoa, focusing on Māori, Pasifika, and Asian communities.
After three unsuccessful research proposals to the Health Research Council, the team used money from the Massey University Research Fund (MURF) to run a pilot study in Porirua, Wellington.
Read British Journal of Cancer article on self testing in the UK
Building on international research
In 2015, the team's Health Research Council application was finally successful (persistence pays off!), for research starting in 2016.
Massey’s Dr Collette Bromhead, an experienced molecular biologist and infectious diseases specialist known informally as the 'High-Priestess of HPV', also came on board.
The Massey researchers drew on research from other countries, including the Netherlands and Australia, where self-testing for HPV has already resulted in higher uptake with women.
This self-testing has led to increased early diagnoses of early-stage cervical cancer, which in turn has led to more lives saved — and fewer lives being disrupted by all the attendant traumas of cancer and treatment (illness, pain, chemotherapy, loss of income, anxiety about the future, and more).
View Doctor Collette Bromhead's research profile
Read about the Netherlands trials
Nationwide trials to test a mana-enhancing procedure
The challenge, in an Aotearoa New Zealand context, was to develop what Māori cervical health advocate Eruera Keepa calls "mana-enhancing" self-testing procedures. In other words, to make self-testing culturally appropriate for Māori and Pasifika women.
In the pilot study, 56 women visiting a Porirua medical clinic were asked to:
- examine three different self-sampling devices
- complete a questionnaire
- take a self-sample with at least one device (of their choice).
The questionnaire was completed face-to-face, followed by self-testing and sample-testing at the clinic. Although it was a small sample size, the results were positive overall. Participants preferring the self-testing process described it "easier" and "comfortable", offering "privacy and convenience"; one participant noted that she’d "rather do it myself".
Brewer, Potter and Co’s larger, HRC-funded, study involved 3,553 Māori, Pasifika and Asian women. These women had either never been screened for cervical cancer or had been ‘under-screened’ (not tested as often as the Ministry of Health recommends). The project was designed to mimic usual clinical practice, thus testing exactly how it could be rolled out.
The findings were conclusive: Māori, Pasifika and Asian women all preferred to self-test, rather than visit the doctor and find themselves in a vulnerable, and potentially alienating, situation. These findings mimic similar results in other countries.
Self test positively received
Māori, Pasifika and Asian women all preferred to self-test, rather than visit the doctor and find themselves in a vulnerable, and potentially alienating, situation.
New Zealand government adopts research findings
Government has been unusually quick to get on-board with the idea. Professor Potter, who has been working in public health for over forty years, was asked if it was common for good new ideas to get picked up so rapidly.
"Rocking horse droppings are a little more common," he replies with a wry grin.
"We designed the experiment to be easily implemented by the government", Potter emphasises. "‘Does this style of self-test make things better – yes or no?' the answer was 'Yes', and bingo: it’s ready to be rolled out. As a researcher, you can come up with all sorts of biological and genetic knowledge, but the question still remains – how to implement it?"
Confirming the importance of this self-testing approach, a 2021 study led by Victoria University Wellington’s Professor Bev Lawton (OMNZ) confirmed "almost 60 per cent of Māori women took the human papillomavirus self-test when offered it – about three times more women than those offered the standard cervical smear."
Self-testing is now set to be made available from July 2023.
"It's an important and exciting breakthrough — it will remove some of the layers of bureaucracy and structural racism that still plague New Zealand’s health system, and help Māori and Pacific women put their health in their own hands."
Planning for impact from the start
Brewer and Potter’s success highlights how thinking about your desired real-world research impact at the very beginning of your project planning can help you produce usable findings. These can be picked up by non-academics – in this case, the Ministry of Health Manatū Hauora – and applied in the real world.
Thanks to the work of Brewer, Potter and their colleagues, under-screened women across Aotearoa will soon be able to take their health into their own hands, administering self-tests. This will reduce illness and death, and potentially help rebuild trust in the health system more generally. As a health researcher, you can’t ask for more than that.
Research Centre for Hauora and Health support
Formerly the Centre for Public Health Research, the Research Centre for Hauora and Health have supported, and continue to support, this research. This includes direct involvement from Neil Pearce, Jeroen Douwes and Chris Cunningham.
Published on 25 January 2022.