Research shows there are a range of reasons why men do not readily address their health needs.
This week is Men's Health Week in Aotearoa New Zealand. I'm sure I've been asked to write this position paper because I am male, a nurse and have spent many years working in mental health.
Awareness weeks are the opportunity to make people aware of challenges associated with the latest problem or celebratory event. Like many countries, New Zealand has more awareness events than weeks in the year. Some address serious topics and some are frivolous, such as 'Loud Shirt Day'. I must admit I like 'National Me Day'. So, in future years, I think I will celebrate that one.
Whether it's a day or a week focussing on an issue, I am unconvinced they make any real difference. The highlighting of challenges, such as getting men to attend to their health needs, doesn’t seem to have resulted in any significant change. Yet, it is true that men's health statistics are concerning.
Statistics show that men in New Zealand are more likely to die by suicide than women, with the suicide rate for men here being three times higher than for women.
Within my own research, there appears to be a range of reasons why men do not readily address their health needs.
I found common themes associated with clinical services having a high threshold for people to access the help needed, for example, not being unwell enough. So, despite in some cases men being desperate for help, they were refused it and referred to other services to be seen for yet another assessment to determine whether they met the 'new service' criteria for acceptance.
People were often left to fend for themselves, communication was poor and they did not know where to turn. Other participants commented that they could not afford to see their general practitioner for any healthcare need, let alone mental health. Their priority is food and rent - healthcare is well down the pecking order.

Philip Ferris-Day.
I recently received various emails and notifications advising about the upcoming Men's Health Week. One contained a brief quiz asking multiple health-related questions. You scored points for the answers, with a summary outlining the meaning of your total score. Unfortunately, despite my relatively healthy lifestyle, I lost points because I have not attended my general practitioner for a wellness check-up, and the recommendation from the quiz was that this needs to be a priority. The reasons were the usual - all associated with men not focusing on their health.
Research has often commented that men's mental health challenges are associated with being strong and stoic and not showing vulnerability or weakness, preventing them from seeking help when needed. Indeed, there may be an element of that, but the actual cost may be the primary factor. It can be somewhat expensive to meet health needs, especially preventative ones.
However, research also indicates some women experience the same challenges as men when seeking mental health support. In my opinion, it is not so much about men but about people, human beings, being connected and belonging. On this note, rather than a Men's Health Awareness Week, can we just have a 'Human Awareness Week'?
Just a thought.
Related news
Mental health help-seeking in men and the role of the media
When a younger Dr Jake Gallagher was struggling with his mental health, he had no idea how to seek help, despite being close to completing a psychology degree. Ten years later, he has just graduated as a Doctor of Clinical Psychology after using his own experience as the motivation for his thesis research.

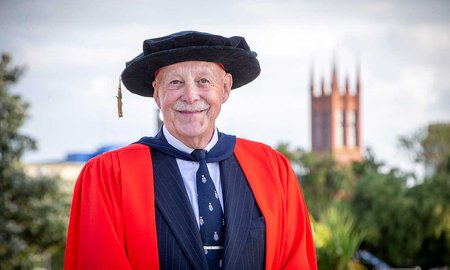
Gay men’s health and discrimination researcher awarded
Massey University alumnus and health psychologist Professor Michael Ross has been awarded a Doctor of Science for his lifetime of research into sexual risk behaviour and mental health in gay and bisexual men across cultures and continents.